194
Ces Urol 2016; 20(3): 192–194
VIDEO
(67.6% of all pRCCs, 6.1% of all renal tumours), the
others were pRCC type 2 (14/148 – 95%), onco‑
cytic pRCC – (opRCC (19–12.8%) and not otherwise
specified (NOS) – (15–10.1%). Oncocytic pRCC has
not yet been officially recognized by WHO clas‑
sification 2016 .
Results:
The preferred method in all groups of
pRCC was resection – in pRCC type 1 up to 80.7%.
For comparison, the ratio of resections performed
during this period of 9 years (1629 tumours) was
48.4%. WHO (ISUP) Grade 1 was most represented
in pRCC type 1. In other groups, Grade 3 was the
most common grade – in pRCC type 2 up to 78.6%.
3-years progression-free survival was 97.1% in our
study, in pRCC type 2 (44,1%), opRCC (85,4%), NOS
(69,9%) (4). The disease progression was observed
in 3 patients with a histologically verified pRCC1. All
3 patients had undergone an open nephrectomy.
In 2 of the cases due to large tumours, 145 and
180mm (stage cT2b and cT3a) and in one case
a tumour duplicity had been diagnosed (tumour
of the sigma). In histologically verified pRCC2, a cy‑
toreductive operation was performed in 2 cases of
progression. In 3 further cases we noted progres‑
sion; of which 2 were after resection and one after
nephrectomy.
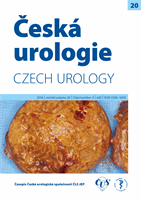
Our video presentation presents a 44years-old,
obese man (BMI 30.8) with a palpable renal tumour
at the lower pole of the left kidney. Tumour size
was 10 cm at the tumour´s widest part according
to CT. The tumour has extrarenal growth, regular
spherical shape, stage cT2a. R.E.N.A.L. score 9a
(6). Translumbal resection was performed, time of
clamping of the hilum 7 minutes and blood loss
100 ml. The tissue sample was ochre coloured,
typically fragile, 639 g and histologically it was
verified as a pRCC type 2, without interference
anywhere in the resection line. The patient is so far
without recurrence of the kidney tumour (period
of monitoring – 32.4 months), but unfortunately
he is being treated for metastatic prostatic cancer.
Conclusion:
Papillary renal cell carcinoma is
possible in most cases safely treated by resection
thanks to its typical extrarenal growth, in individual
cases also in stage cT2a. It is necessary to closely
monitor patients after resection with histologi‑
cally verified pRCC type 2 tumours for their proven
higher potential of malignancy.
KEY WORDS
Grade, papillary renal cell carcinoma, obesity, prog‑
nosis, resection.
LITERATURA
1. Hora M, Hes O, Boudová L, et al.
Papilární renální karcinom. Ces Urol 2002; 6: 26–31.
2. Hora M, Hes O, Klečka J, et al.
Rupture of papillary renal cell carcinoma. Scand J Urol Nephrol 2004;
38: 481–484.
3. Delahunt B, Eble JN, McCredie MRE, Bethwaite PB, Stewart JH, Bilous AM.
Morphologic typing of
papillary renal cell carcinoma: Comparison of growth kinetics and patient survival in 66 cases. Hum Pathol
2001; 32: 590–595.
4. Procházková K, Staehler M, Travníček I, et al.
Morphological Characterization of Papillary Renal Cell
Carcinoma Type 1, the Efficiency of its Surgical Treatment. Urol Inter 2016 in print, DOI: 10.1159/000448434
5. Delahunt B, Eble JN.
Papillary renal cell carcinoma: a clinicopathologic and immunohistochemical study
of 105 tumors. Mod Pathol Off J U S Can Acad Pathol Inc 1997; 10: 537–544.
6. Kutikov A, Uzzo RG.
The R.E.N.A.L. Nephrometry Score: A Comprehensive Standardized System for
Quantitating Renal Tumor Size, Location and Depth. J Urol 2009; 182: 844–853.